Glaucoma, by definition, is a group of eye diseases that cause optic nerve damage. Glaucoma causes loss of vision—first affecting the periphery and progressing towards the centre of vision. This means a person can still see what they are staring at, but areas outside the central concentrated spot slowly disappear.
Glaucoma affects one eye more than the other, so one eye may be doing great and sees everything while the other eye is slowly becoming blind.
To understand the causes of glaucoma, we have to look at the anatomy of the eye.
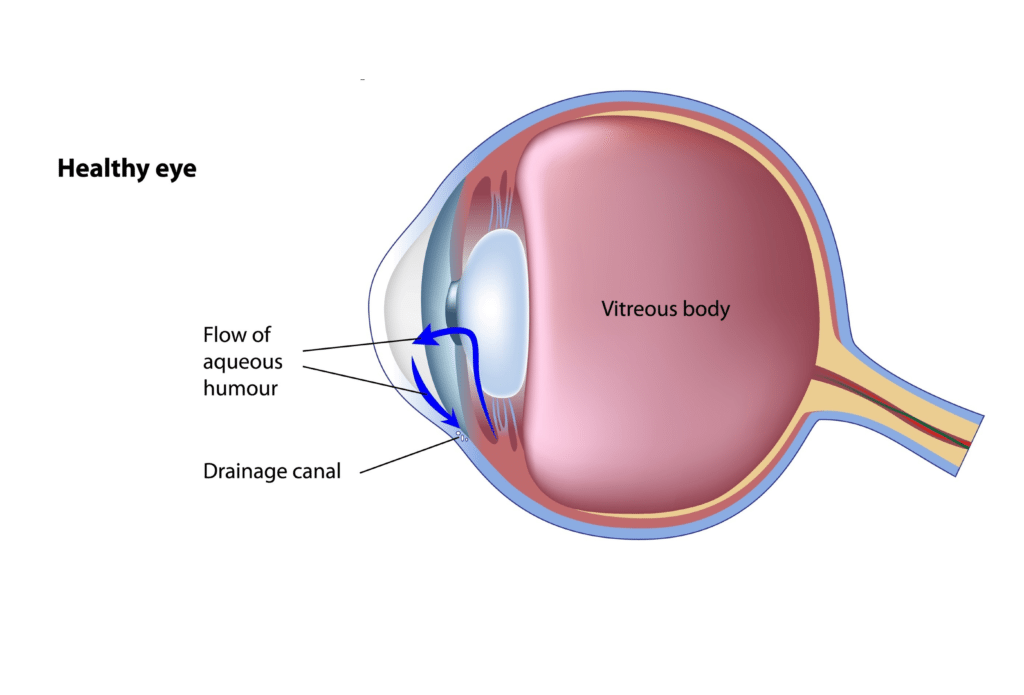
In a healthy eye, a clear liquid called the aqueous humour is released and circulates to the front portion of the eye. An equal amount of this fluid leaves the eye through the drainage canal. This inflow and outflow gives the eye a balanced internal fluid pressure to retain its globular shape and the ability to see well.
 Elevated Eye Pressure
Elevated Eye Pressure
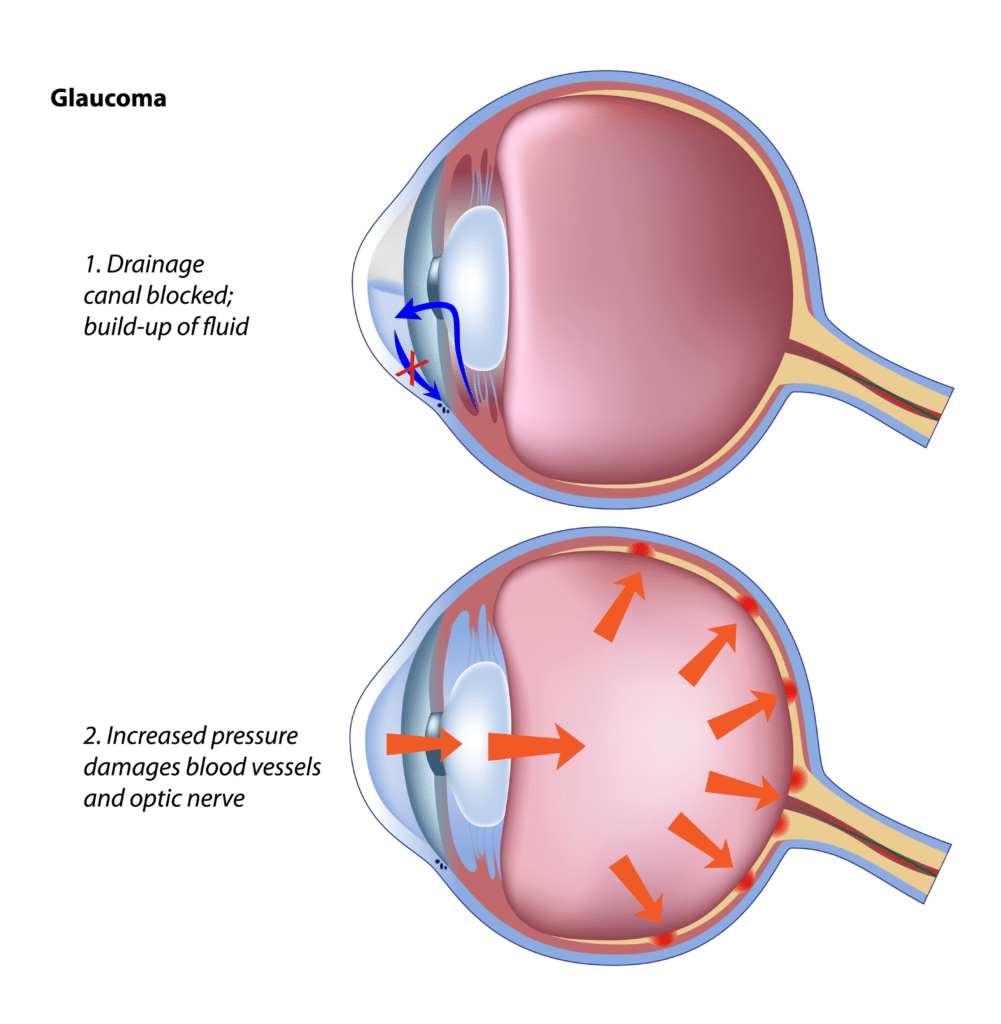
When the eye’s fluid does not flow through the drainage canal properly, fluid accumulates in the eye causing an elevated eye pressure. This extra force is believed to compress the optic nerve in the back of the eye, causing damage to the delicate optic nerve fibres. As nerve fibres get damaged, vision is lost.
Dr Alexander Du, optometrist at Eyecare Plus Kareela, states, ‘Initially it was thought glaucoma was caused solely by an increase in IOP (intraocular pressure). Yes an increase in IOP does cause faster deterioration, but there are many patients whose IOP is within what’s classified the ‘normal range’ of 9-21mmHg who still progress. High and low blood pressures have also been linked to glaucoma, however eyecare providers are still coming to terms on why this is the case.’
Congenital
‘Congenital cases are unlike “normal glaucoma” because they happen at birth due to defects in the formation of the eye. It is completely different to age related glaucoma that occurs due to changes in the physiology of the eye as you age. Congenital cases are normally detected by the paediatrician during their normal checks within the first few months of birth,’ Alex Du continues.
Secondary to Other Eye Conditions, Injuries or Surgeries
‘Some eye conditions can impact on the IOP of the eye and in turn cause glaucoma. Glaucoma can happen because of something as simple as a cataract; in-fact the most common cause of increased pressure in the eye is due to a dense and thick cataract lens. This cataract lens hinders the outflow of the aqueous humour and hence causes the pressure to go up. According to the Ocular Hypertensive Study, the removal of a cataract can reduce IOPs by 4-5mmHg,’ states Alex Du.
‘Any trauma in the eye due to an eye injury can present itself anywhere down the track from a few weeks to tens of years away. Trauma can cause what’s known as angle recession which reduces the flow of the aqueous humour out of the eye.’
‘Surgeries involving the eye will normally require anti-inflammatory eyedrops post-surgery which can cause pressure spikes in some individuals.’
Optic Nerve Damage
The optic nerve is a cable of delicate nerve fibres that carry electrical impulses from the eye to the brain. Not only are they delicate, but they do not have the capacity to regenerate or heal themselves; hence damage to the nerve fibres are permanent. No one knows the exact reason why the optic nerve gets damaged without reports of shock, toxins, radiation or trauma. It could be that some individuals optic nerves are more sensitive than others or there is less blood being supplied to the optic nerve.
Alex Du states, ‘Optic nerve head damage is the pinnacle of glaucoma. Patients can have low pressures yet still have optic nerve head damage and be considered to have glaucoma. However, if pressures are above the “normal” range, with no optic nerve head damage, then they are merely glaucoma suspects.’
Our Optometrists’ Role in Screening and Co-managing Patients with Glaucoma
Eyecare Plus Optometrists providing Eyecare Vision services have advanced diagnostic equipment used to screen for glaucoma and other eye diseases.
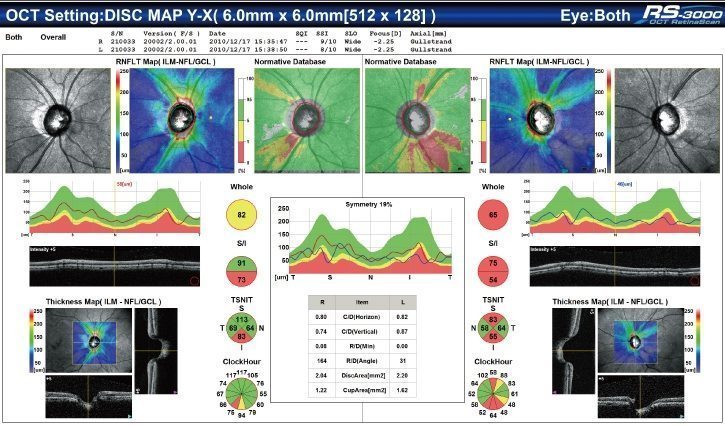
Alex Du states, ‘All our optometrists have access to an OCT (optical coherence tomography), stereoscopic retinal imaging, gonioscopy, applanation tonometry, and central corneal thickness measurements which allow us to monitor and diagnose glaucoma as early as possible.’
If you are found to have glaucoma, our optometrists will refer you to an eye specialist who will make a treatment plan and may co-manage your condition with the optometrist.
‘All therapeutically endorsed optometrists are recognised as being able to adequately co-manage patients with glaucoma. They can prescribe all the necessary drops required for glaucoma treatment and are usually the first to see a patient who is developing glaucoma,’ states Alex Du.
